Dr Jeff Moore, Director of Research Jigsaw
Data, Decisions, and the Bigger Picture
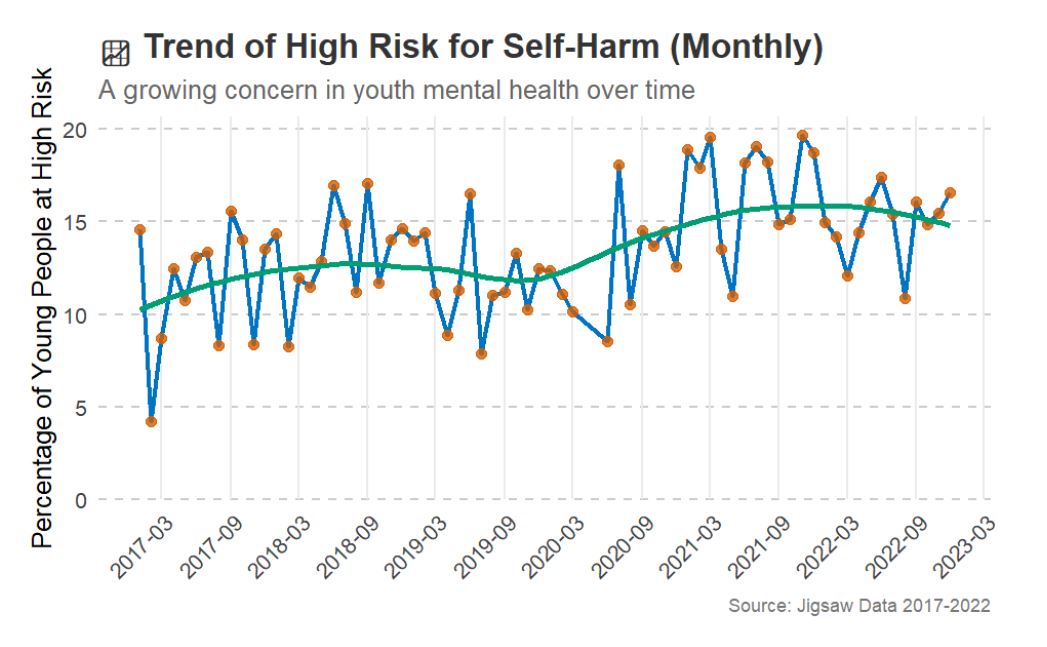
Data tells stories. In healthcare, it helps us see patterns, understand trends, and figure out what’s working—and what needs to change. When it comes to youth mental health, this is more important than ever.
Every young person who reaches out for support has their own unique story, and those individual experiences matter. At the same time, data allows us to step back and see the bigger picture—helping us understand who is accessing support, where gaps exist, and how we can improve services to meet growing demand.
Young people today are facing huge challenges, and we know that most mental health difficulties start before the age of 25. That’s why early support is critical. But are young people getting the help they need? Who is reaching out for support? And once they do, what keeps them engaged—or causes them to drop out?
Since 2006, Jigsaw has been offering free, accessible mental health support to 12- to 25-year-olds in Ireland. To get a clearer picture of how the service is being used, we dived into five years of data (2017-2022). Here’s what we found.
More Young People Reaching Out
Over these five years, nearly 29,000 young people sought support from Jigsaw. That’s a lot of young people looking for help, and the numbers kept growing. More referrals have come from family members, teachers, and GPs, showing that young people aren’t the only ones recognising the need for mental health support—those around them are stepping up too.
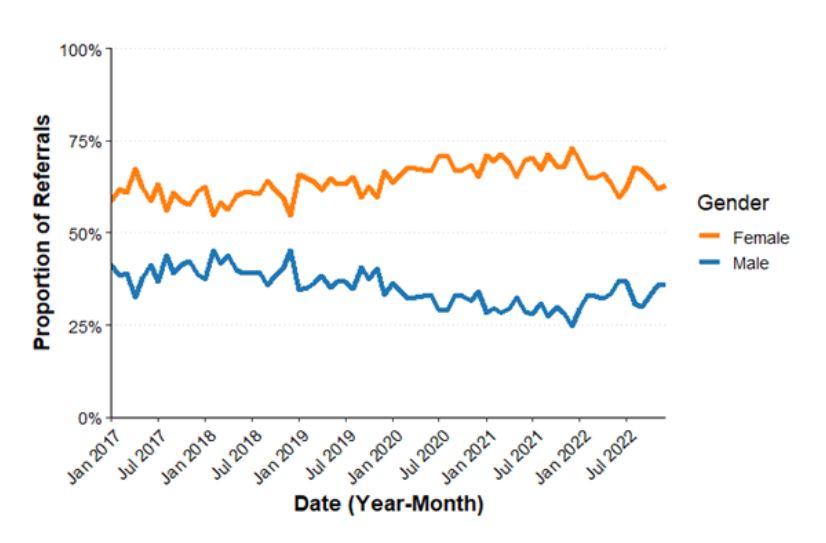
One notable improvement is the increase in male referrals over time. While young women still make up the majority of referrals, we’ve seen a steady rise in young men seeking support, which is an encouraging shift. This suggests that awareness and accessibility efforts may be helping to break down some of the barriers traditionally preventing young men from engaging with mental health services.
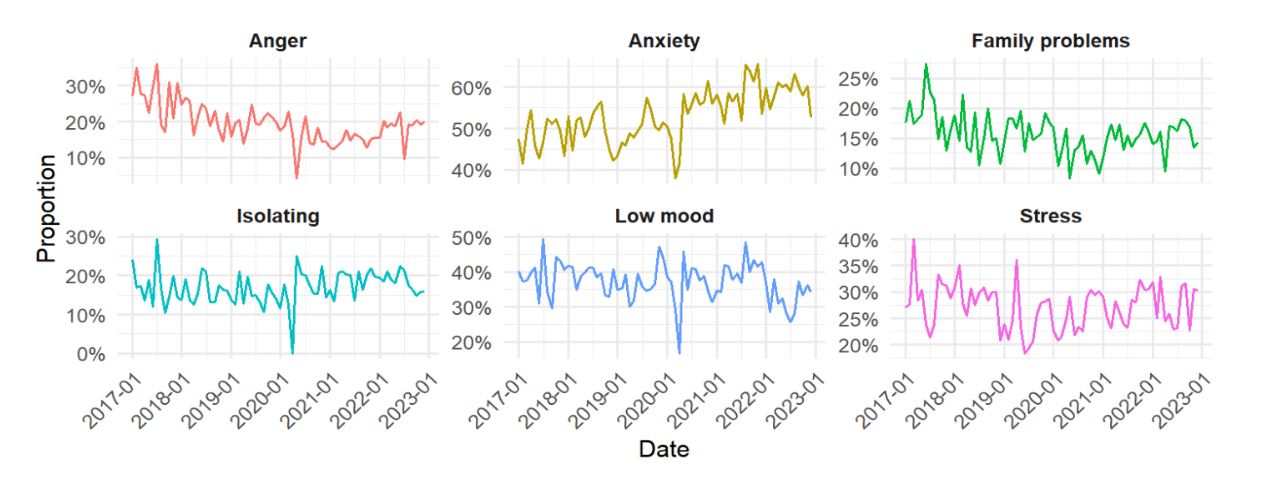
So, who’s the average Jigsaw user? They’re 16 years old, most likely female, and struggling with anxiety. Anxiety was by far the most common reason young people sought support, followed by low mood and stress. In fact, anxiety-related presentations increased significantly over the five years, reflecting wider concerns about youth mental health globally. But while demand was rising, so were wait times.
Who’s Attending, and Who’s Dropping Out? Who’s Attending, and Who’s Dropping Out?
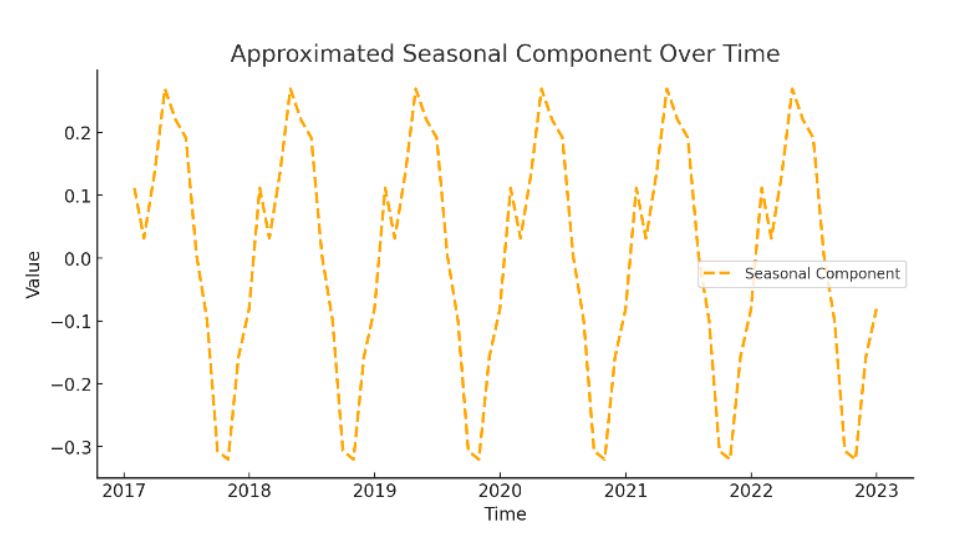
Not everyone who reaches out for support stays engaged. On average, young people attended six sessions, but some came for just one, while others completed the full program. Gender played a role—young men were less likely to stick with it. Anxiety kept young people engaged, but severe distress, especially for 17- to 25-year-olds, made it harder to continue. Referral source mattered too—those referred by parents stayed engaged more than those referred by schools or GPs. Timing also played a part, with more young people starting therapy in January and September, but engagement dipping in June and December.
Moving Forward: Strengthening Youth Mental Health Support
Expand Access to Brief Interventions:
To meet increasing demand, we need continued investment in short, targeted interventions that provide immediate support while ensuring resources remain available for those who need longer-term care.
Develop Tailored Engagement Strategies for Young Men:
With young men likely to attend fewer sessions we must rethink how services are delivered—offering less formal, more practical, and accessible formats that meet their unique needs.
Strengthen Family and Community Involvement:
Since family referrals improve engagement, we should focus on empowering parents and caregivers with tools and knowledge to support their child’s mental health journey. Schools, youth organizations, and communities must also play a stronger role in early intervention.